Beneath the warmth of the sun’s rays lies a vital nutrient that quietly shapes the foundation of our well-being: vitamin D. Frequently enough celebrated for its role in strengthening bones, this essential vitamin also plays a less visible yet equally crucial part in maintaining heart health. As the bridge between sunlight and our body’s intricate systems, vitamin D stands at the crossroads of skeletal strength and cardiovascular resilience. Exploring this multifaceted vitamin reveals a deeper understanding of how we might nurture not just our bones, but the very rhythm of life itself. in this article, we delve into the remarkable role of vitamin D in supporting both bone and heart health, uncovering the science behind its impact and why it deserves a central place in our wellness conversations.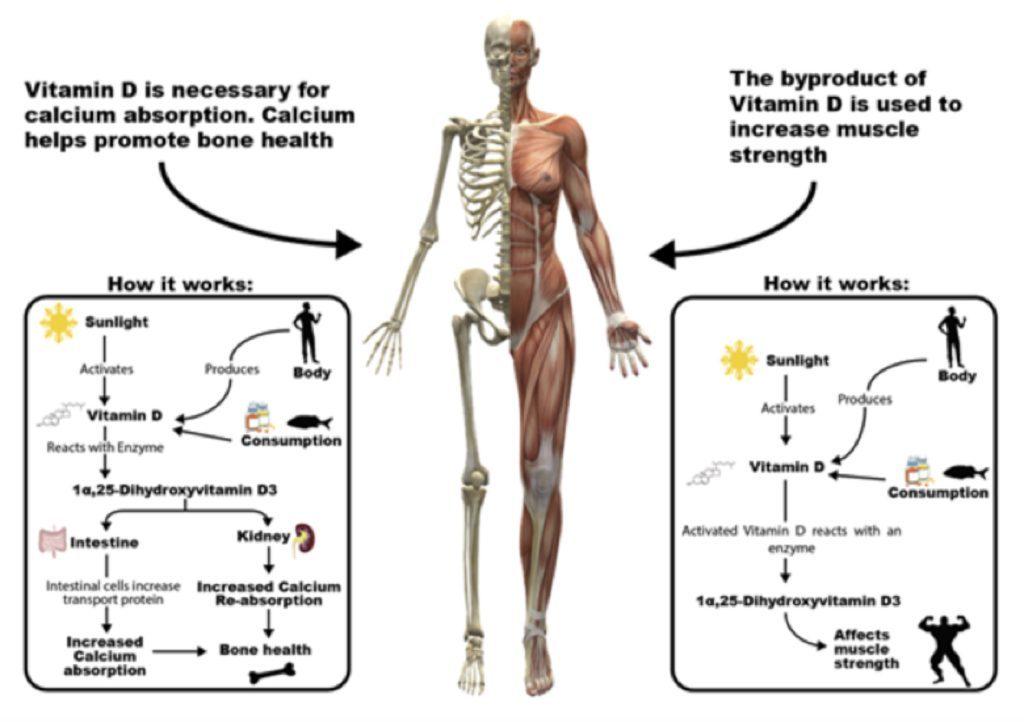
The Impact of Vitamin D on Bone Density and Fracture Prevention
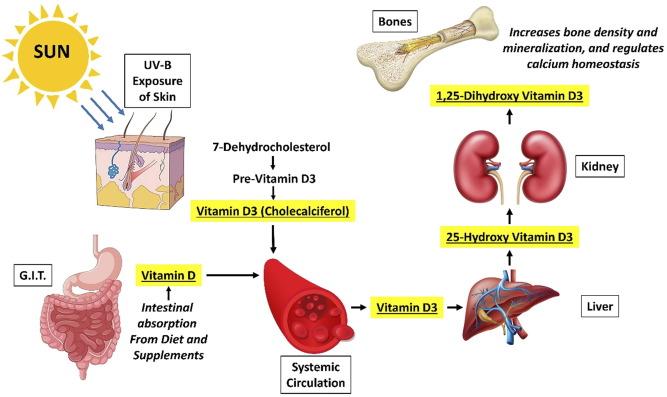
Vitamin D plays a pivotal role in maintaining optimal bone health by facilitating calcium absorption in the gut, which is essential for bone mineralization and strength. Insufficient levels of this vital nutrient can lead to decreased calcium absorption, prompting the body to leach calcium from bones to maintain blood calcium levels. This process ultimately results in weakened bone structure, increasing susceptibility to conditions like osteoporosis and elevating fracture risk, especially in older adults. Research consistently highlights the necessity of adequate vitamin D for preserving bone density and reducing the incidence of fractures linked to falls.
Key benefits of vitamin D for bone health include:
- Enhancing calcium uptake to support bone remodeling
- Promoting muscle function,thereby aiding balance and preventing falls
- Reducing inflammation that may compromise bone integrity
The synergy between adequate vitamin D levels and bone mineral density is well-documented,with global health authorities such as the National Institute of Arthritis and Musculoskeletal and Skin Diseases emphasizing supplementation in at-risk populations. Below is a summary of recommended serum 25(OH)D levels and their corresponding impact on fracture risk:
| Serum 25(OH)D Level (ng/mL) | Fracture Risk Reduction |
|---|---|
| Less than 20 | High risk |
| 20–30 | Moderate risk |
| Above 30 | Lowest risk |
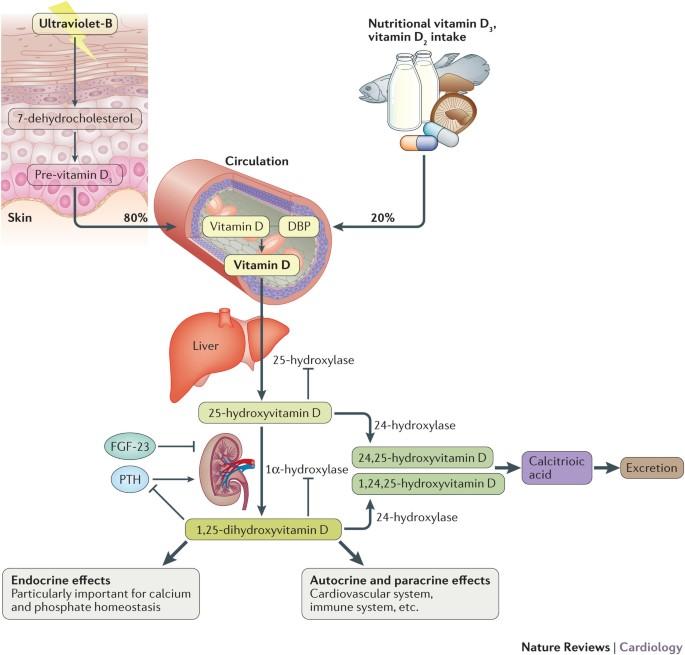
Exploring Vitamin D’s Influence on Cardiovascular Function
Vitamin D, often celebrated for its pivotal role in bone health, also casts a significant influence on cardiovascular function. Research increasingly reveals that this nutrient is more than a bone-builder; it acts as a modulator of heart muscle performance, blood pressure regulation, and vascular health. A deficiency in vitamin D has been linked to increased risks of hypertension,heart failure,and coronary artery disease,hinting at its crucial role in maintaining the elasticity and function of blood vessels. This happens because vitamin D receptors are present in heart cells and vascular smooth muscle,enabling it to directly impact cardiovascular physiology.
Key mechanisms through which vitamin D supports heart health include:
- Regulating inflammation: Vitamin D helps reduce the release of pro-inflammatory cytokines, which are known contributors to atherosclerosis.
- Modulating the renin-angiotensin system: This hormone system controls blood pressure and fluid balance, with vitamin D acting as a suppressor that prevents excessive pressure build-up.
- Supporting endothelial function: Ensuring that the lining of blood vessels stays healthy, which is essential for preventing clot formation and maintaining smooth blood flow.
| Vitamin D Cardiovascular Effect | Potential Outcome of Deficiency |
|---|---|
| Anti-inflammatory response | Chronic vascular inflammation |
| Blood pressure regulation | Hypertension |
| Endothelial cell health | Increased risk of arterial stiffness |
Those interested in deepening their understanding of vitamin D’s cardiovascular benefits can explore scientific resources such as the American Heart Association and detailed vitamin D studies available through the National Institutes of Health.These institutions offer comprehensive insights that can empower informed health decisions based on the latest research.
Balancing Sun Exposure and Dietary Sources for Optimal Vitamin D Levels
Striking the right balance between sun exposure and dietary intake is essential to maintain optimal vitamin D levels without risking skin damage. While sunlight triggers the synthesis of vitamin D in the skin, factors such as geographic location, skin pigmentation, and the use of sunscreen can considerably influence the amount produced.Experts generally recommend about 10 to 30 minutes of midday sun exposure several times a week, but this varies from person to person. Overexposure, however, can lead to harmful effects such as sunburn and increased risk of skin cancer, underscoring the importance of moderation and protection.
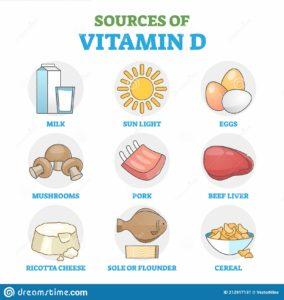
Complementing sun exposure with a nutrient-rich diet helps secure adequate vitamin D, especially during the winter months or for those with limited outdoor activity. Incorporating foods like fatty fish, fortified dairy products, and egg yolks can naturally boost intake. here’s a speedy guide to some vitamin D-rich foods:
| Food | Vitamin D (IU per serving) |
|---|---|
| Salmon (3.5 oz) | 570 |
| Fortified Milk (1 cup) | 120 |
| Egg Yolk (1 large) | 40 |
| Mushrooms exposed to UV (3.5 oz) | 450 |
- National Institutes of Health provides comprehensive dietary recommendations.
- For detailed guidance on sun exposure, CDC’s sun safety tips are invaluable.

Tailored Vitamin D Supplementation strategies for Bone and Heart Health
personalized vitamin D supplementation is quickly becoming a cornerstone in optimizing bone and cardiovascular health. Individual needs vary significantly based on factors such as age, geographic location, skin pigmentation, and existing health conditions. As a notable example, older adults and individuals with limited sun exposure frequently enough require higher doses to maintain serum 25(OH)D levels within the optimal range of 30-50 ng/mL. Meanwhile, patients with cardiovascular risk factors may benefit not only from adequate vitamin D to support calcium metabolism but also for its potential anti-inflammatory and endothelial function benefits. Tailored approaches ensure supplementation is effective without risking hypervitaminosis D or related complications.
When designing supplementation plans, healthcare providers frequently enough consider these key elements:
- Baseline Vitamin D Status: Steadfast through serum testing to customize dosing.
- Lifestyle Factors: Including diet, sun exposure, and physical activity.
- Concurrent Medications or Conditions: To avoid interactions and optimize metabolism.
| Group | Typical Dose | Supplement Duration |
|---|---|---|
| Adults with Deficiency | 1,000–2,000 IU/day | 3–6 months |
| Older Adults | 800–1,200 IU/day | Ongoing |
| Cardiovascular Risk Patients | Reviewed case-by-case | Monitored quarterly |
For a thorough understanding of vitamin D’s clinical applications, the NIH Office of Dietary Supplements offers extensively researched guidelines. Additionally, emerging evidence compiled by the American Heart Association highlights the meaning of individualized vitamin D strategies in reducing cardiovascular disease risk.
The Way forward
As the sun’s gentle rays continue to weave their way through our lives, vitamin D quietly works behind the scenes—fortifying bones and supporting the steady rhythm of the heart. While it may not steal the spotlight like some nutrients, its role is undeniably vital. Embracing a balanced approach to vitamin D intake, whether through mindful sun exposure, diet, or supplementation, can be a subtle yet powerful step toward overall wellness. In the intricate dance of health, vitamin D reminds us that sometimes, the simplest elements hold the greatest strength.